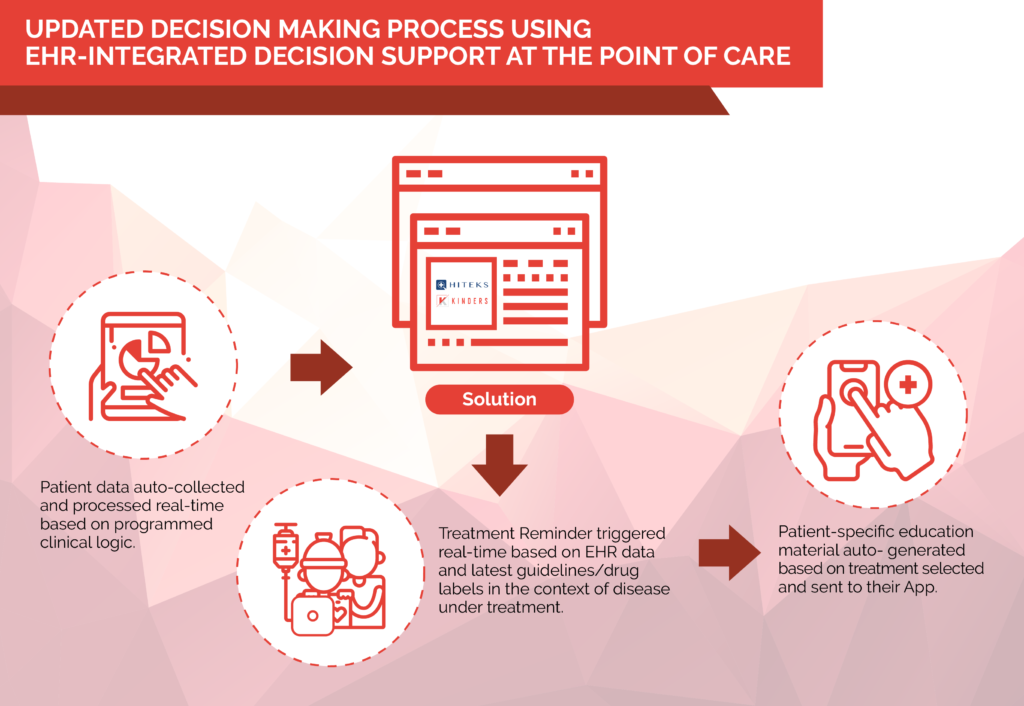
Digital workflows now allow for the ongoing support of clinicians at the point of care, using a combination of well-designed technical solutions and clinical logic that’s based on patient data and the application of guidelines and drug labels.
The trouble with pharma marketing
For years, Big Pharma has marketed its drugs to healthcare providers using a tried-and-true model: running clinical trials, publishing the results in journals, and presenting them at conferences. To drive awareness, brands leverage the evidence in marketing campaigns and physician detailing.
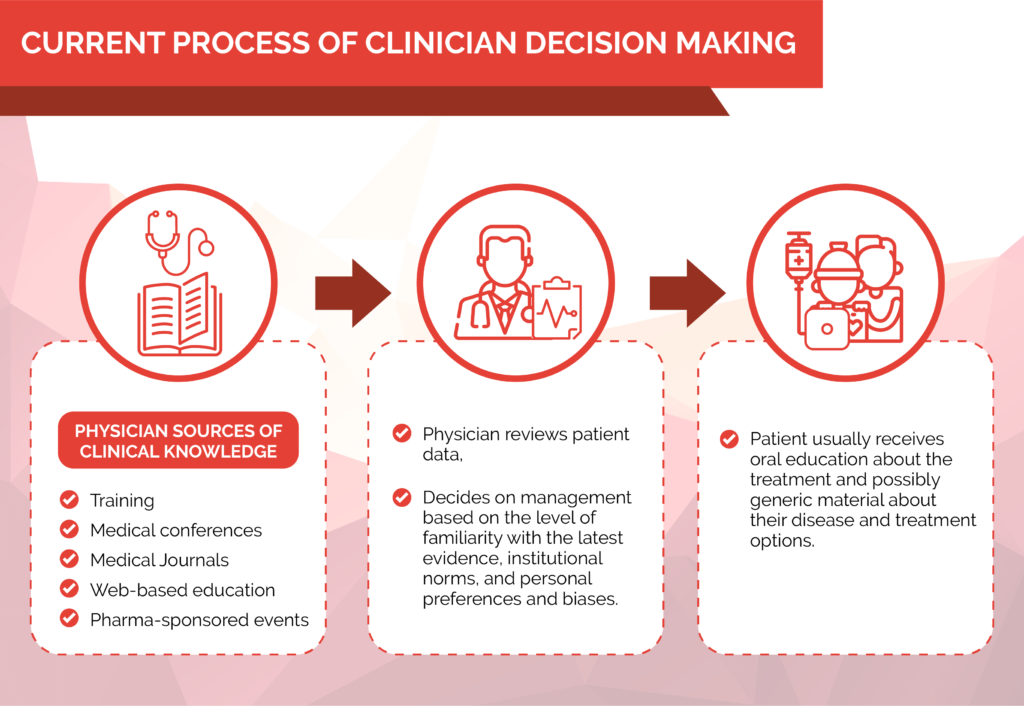
Ubiquitous as it’s become, however, this approach is becoming less and less effective as the treatment options expand and it becomes harder for the physicians to remember all of this information. In many cases, brands underperform because physicians continue to use older and cheaper alternatives, even when a brand offers significant advantages in certain patient populations.
In other cases, several drugs are indicated to treat a single illness, and physicians do not remember the nuances of each alternative at the point of care. Increasingly important are the workflow distractions of the practicing physician; most of their time is now spent in the digital environment reviewing or entering patient data.
Clinical decision support: the opportunity
So, how do you overcome this issue? By spending even more on physician education to cover every possible clinical scenario and which treatment to use in each? Perhaps. Improving physician education is always a worthy goal. But brands reach a point of diminishing returns when it comes to information retention: physicians simply won’t remember each detail, in each scenario, at the point of care. eDetailing, in which interactive digital content is made available for clinicians to review on their own time, has drawn a positive response, but information about ROI is still limited. But again, no matter how the information is delivered to the physicians, the key issue is for them to remember it at the point of care when choosing between very similar therapies with only subtle differences in certain patient populations.
Some of the developments of the last decade offer a new path forward. In recent years, the adoption of Electronic Health Records (EHR) has significantly increased. The newest EHRs have improved functionalities, making relevant clinical information like radiology, pathology, and labs more easily available within the system. Given that clinical workflows are already increasingly digital, there is a natural opportunity to educate physicians about possible treatment options at the point of care, rather than before or after it.
Challenges with POC Support tools
What, then, is keeping point-of-care education and decision support from being widely used today? The answer is that although many things are possible in theory within EHRs, the reality is a long way from this theory. One of the key barriers is the difficulty of interfacing with EHRs. There are many reasons for this. EHR companies create obstacles to prevent access to their proprietary databases. Medical centers, meanwhile, have a high number of competing projects. Finally, nearly 80% of the data in EHRs is unstructured, meaning it must either be ignored or—often manually—converted before it’s accessible and available for analysis.
These barriers would give pause to any Life Sciences company. Indeed, they are some of the primary reasons that the ROI for such projects to date has been unfavorable.
However, they are not insurmountable, as we discovered when we began to devise a business process and technology solution that could anticipate and overcome them. In fact, our experience building Kinders and Hiteks—two companies that leverage new technologies and enhance healthcare business models—suggests that with the right tools and workflows, Life Science companies can build point-of-care solutions that are highly effective marketing vehicles.
Evaluating point of care support tools
Here’s what companies should look for as they evaluate potential partners and systems:
- EHR integration: It’s no secret that the EHR landscape is complex and cluttered. But your installation costs will skyrocket if your point-of-care solution doesn’t easily integrate with the EHRs that are being used at the majority of medical centers. For Hiteks, we first built software that would integrate easily into of most major commercially available EHRs, especially Epic. Then, we fully integrated this into the Epic main engine to become an application for their customers. Because Epic has the largest base of users, this allows us to achieve the wide-scale adoption of new decision support solutions without additional local installation—and create a turnkey solution on the technical side.
- Effective methodology: False positives and irrelevant suggestions are a big problem in POC support. To minimize override rates, make sure providers at the health systems that you are implementing work with you to create decision support that results in highly relevant reminders based on their own workflows. Our approach includes studying the clinical guidelines and drug labels for the brand, understanding current institutional clinical decision making around the specific illness, mapping current workflows within the EHRs, clearly defining the pivotal points in decision process, and building logic to generate reminders at the right time.
- ROI measurement tools: You won’t be able to improve your POC support tools—or make the case for extending them to other brands—unless you keep rigorous track of your results. By combining software that’s fully integrated into the EHR and a robust clinical logic creation methodology, our software can launch point of care decision support reminders quickly and consistently. We then closely monitor engagement with our reminders, using EHR logs to track clinicians’ acceptance of the advice—and any resulting behavioral changes.
Case study: Putting POC tools to the test
Our experience shows that point-of-care support solutions can be highly effective. One pharma brand we worked with had a novel treatment in sepsis. Yet while clinical evidence showed significant advantages for their treatment in certain patients—reducing progression from Sepsis and Severe Sepsis to Septic Shock by 25% and shortening the length of stay by half a day—72% of physicians continued to rely on commonly used antibiotics that have been the mainstay of sepsis treatment for decades.
After careful study of the clinical workflows and clinician decision-making process, we identified all of the key data elements that clinicians use in choosing a sepsis therapy. We then mapped where each one of these data elements resides in the EHR. Using the most up-to-date clinical guidelines and the drug label, we created the logic to generate a reminder in the EHR for the clinicians at the appropriate moment during the management process. This guidelines-based reminder showed the benefits of the novel therapy for the appropriate patients. The reminder was brief, cited the evidence, and allowed the physician to click on the reminder and prescribe the medication.
These are key elements for the success of POC decision support: only generating the reminder at the appropriate moment in the management process; avoiding lengthy narratives that the physicians don’t have time for; highlight the key evidence supporting the reminder; and allow for an easy workflow for them to act on the reminder. Within 12 months, this solution led to 27% increase in the usage of the therapy as the first line of treatment.
Written by Ronald M. Razmi, MD, and Gerry Petratos, MD
Get the Skills You Need
Thousands of independent consultants, subject matter experts, project managers, and interim executives are ready to help address your biggest business opportunities.
About the Author
More Content by Ronald M. Razmi, MD